Traditional plaster casting is still the primary way patients are fitted with prosthetics. It involves measuring partial limbs manually, applying uncomfortable layers of plaster, and waiting for it to dry. In many cases, the resulting casts aren’t stored, meaning that measurements that could still be valuable later on are lost. The plaster simply becomes waste.
3D scanners can make prosthetic customization far less invasive and easier for clinicians. And when coupled with AI software, patients can receive better devices faster.
These were the findings from a study by the Thomas More University of Applied Sciences in Belgium and Orthobroker, which designs and manufactures patient-specific orthoses using 3D printing technology.

Digitizing Prosthetic Design
Working from their base in the Belgian city of Geel, the University’s Mobilab & Care lab team works to improve the quality of life for those with care or support needs. Over the last 16 years, they have investigated the way orthopedics and patients interact to uncover new approaches to creating better-tailored devices.
Using advanced technologies, including 3D scanning and 3D printing, the team digitizes the process of tailoring prosthetics, sockets, and limbs to patients, allowing them to be designed with greater creative freedom, and manufactured much more quickly.

The Mobilab & Care crew has been able to strike many partnerships with orthopedic firms, hospitals, and academic institutions to put their ideas to the test. So far, these projects have taken place in both clinical and scholarly settings, and seen the researchers work with clinicians and patients to develop custom prostheses and orthoses for hands, wrists, and other affected limbs.
Early on in these initiatives, Tom Saey, Mobilab & Care researcher and business developer, says they identified a gap in the market between the 3D scanners most often applied by clinicians and what they actually needed.
“We noticed that within the orthotic industry, they’d been using 3D scanners for some time, only not to 3D print orthoses, but mill positive models instead,” Saey says. “But back then, most of the scanners used were sold by the suppliers of these milling systems and the software that came with them. We also looked at these scanners but soon ran into limitations.”
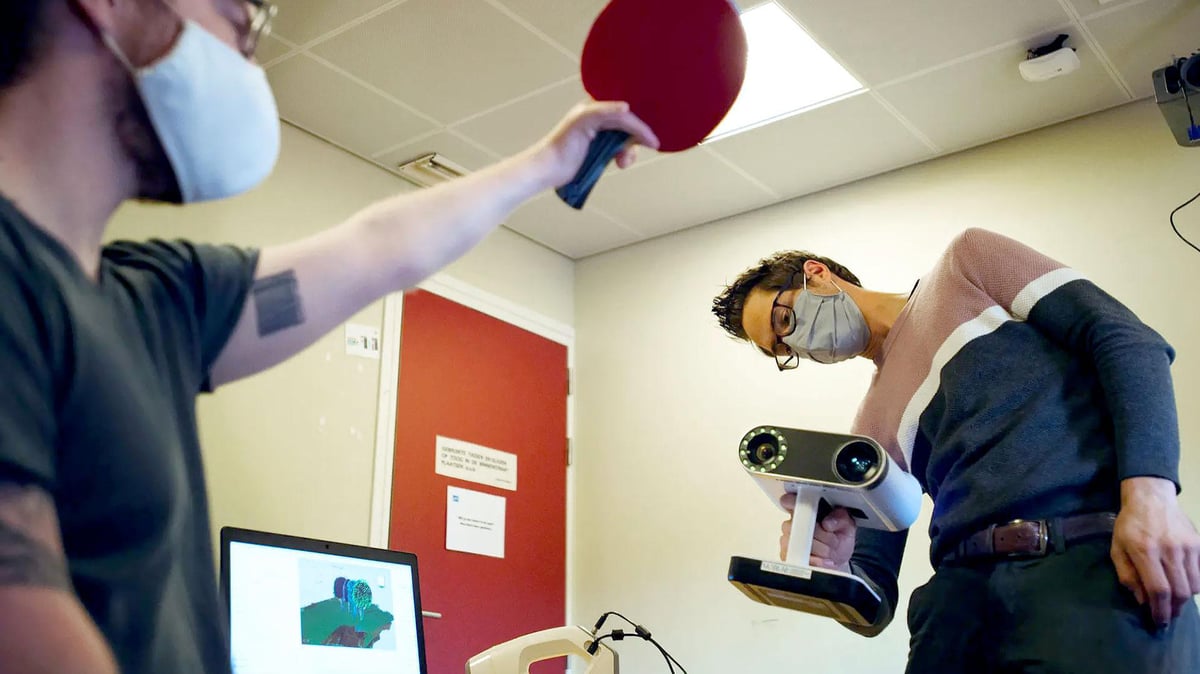
Based on their findings, Saey and his colleagues sought a more capable alternative. At first, his team had success limb-scanning with the Artec Eva, but Saey says it was clear that a wireless solution would have more benefits. They then moved to the AI-powered wireless Artec Leo with a built-in display.
“When we used wired scanners with students, we noticed that looking at a computer screen while you scan makes it difficult,” says Saey. “For a lot of people, that’s a big disadvantage. Also, if you’re scanning patients and you need to move around them, it’s always easier to do so when you have no wires. Those are the two main reasons we adopted Leo.”
The advantage of using a scanner to take accurate measurements is that there is no need to touch the patient at all. The contact-free nature of 3D scanning makes it ideal for switching from messy casting to digital measurement.
Automate Scanning with AI
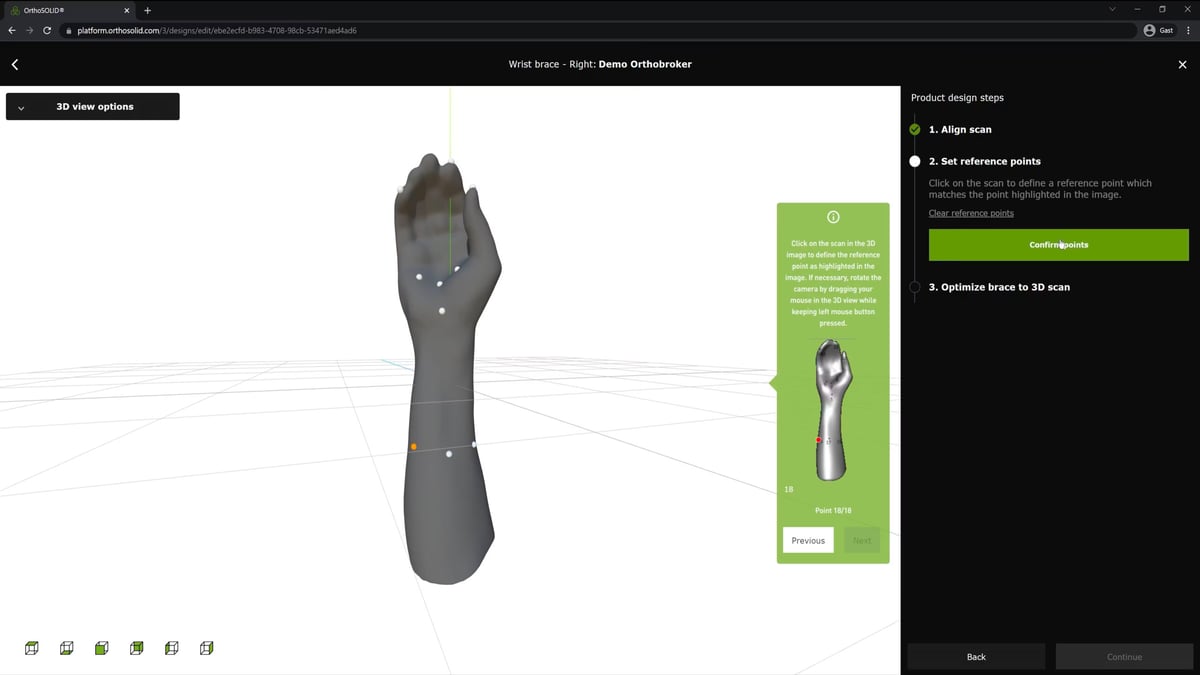
After adopting Artec Leo, the Mobilab & Care team began work with Orthobroker to develop a predictive model for designing lower limb prosthetics. According to Saey, these devices currently need to be “designed from scratch” each time, in a process that requires “a lot of CAD software operations” and manual corrections.
However, as the vast majority of these changes are similar for many patients, the researchers’ AI algorithm is said to be capable of predicting and making changes automatically.
So, how did the software learn how to do this? That’s where Artec 3D scanning came into play.
With both their Eva and Leo scanners, the team was able to accurately capture the bodies of a large group of amputees. They then exported the resulting 3D meshes to Rhino 3D, a CAD software best known for its freeform modeling tools. Once imported, the models’ key features were extracted and used to train their predictive prosthesis customization model.
Though still under R&D by Orthobroker, it’s said that once finished, the algorithm will be integrated into a platform that can be used to accelerate prosthetic socket design.
“What clinicians normally do is make corrections to a mold before they use it to make the final prosthetic. But 95% of the corrections they do are similar in many patients,” says Saey. “We set out to predict these just based on the scan of the patient’s stump and some other parameters. This way, we can avoid the traditional need to spend hours in front of a computer, and they can still make small, patient-specific changes themselves.”
While Orthobroker continues to fine tune this AI-led predictive model, the Mobilab & Care team has resumed its hunt to find further ways of improving life for amputees everywhere. When it comes to 3D scanning, Saey claims the technology has an important role to play in this, but he says devices need to be quick, accurate, and easy to pick up, to find widespread adoption.
Moving forward, Saey believes that 3D scanners have strong credentials as a prosthetic customization tool since it can measure patients’ bodies with a level of speed and accuracy that is unmatched by the devices clinicians currently use.
“What we see in the sector is that a lot of companies look at cheaper alternatives, but they need to know the downsides of these because you can’t expect to get the same high-quality scans from them,” says Saey. “If you need accuracy, it’s important to use a decent scanner because if you intend to 3D print devices but start with a bad scan, your outcome will be bad as well. So I think weighing this up is an important first step.”
License: The text of "AI & 3D Scanning Automates, Accelerates Prosthetic Customization" by All3DP Pro is licensed under a Creative Commons Attribution 4.0 International License.

